Emerging Therapies for Obesity: A Comprehensive Review of GLP-1 Receptor Agonists and Dual Agonist Agents in Phase 3 Clinical Trials
Abstract:
Obesity is a global health challenge associated with significant morbidity and mortality, particularly due to its links to cardiometabolic diseases. Pharmacotherapy targeting the gut-brain axis, specifically glucagon-like peptide-1 receptor agonists (GLP-1 RAs), and combination therapies involving amylin analogs or glucagon receptor agonists, have emerged as potent interventions. This review summarizes the current landscape of anti-obesity agents undergoing phase 3 clinical trials, including novel GLP-1 RAs (orforglipron, ecnoglutide, TG103), GLP-1 RA plus amylin analog (CagriSema), and dual GLP-1/glucagon receptor agonists (mazdutide, survodutide). We detail the pharmacological profiles, clinical efficacy, and safety data available, highlighting the potential of these agents to transform obesity management.
Keywords:
Obesity, GLP-1 receptor agonists, glucagon receptor agonists, amylin analog, weight loss, clinical trials, CagriSema, orforglipron, mazdutide, survodutide
Introduction:
Obesity prevalence has reached epidemic proportions globally, necessitating effective treatment options beyond lifestyle interventions. Pharmacological strategies targeting gut-derived hormones have demonstrated significant weight loss and metabolic benefits, particularly GLP-1 RAs. More recently, novel combinations and dual agonists harnessing multiple pathways (GLP-1, glucagon, and amylin) have shown synergistic effects on weight reduction and metabolic health. This review focuses on anti-obesity pharmacotherapies in phase 3 development, summarizing the latest data on their mechanisms, efficacy, and ongoing research.
GLP-1 Receptor Agonists in Phase 3 Development
1.1 Orforglipron
Orforglipron (LY3502970) is a potent oral, nonpeptide partial GLP-1 RA with preferential cAMP activation over β-arrestin recruitment, potentially reducing receptor desensitization. Its half-life ranges from 28.7 to 49.3 hours, supporting once-daily dosing without food restrictions.
In a phase 2 trial (n=272), orforglipron at doses of 12–45 mg daily for 36 weeks resulted in dose-dependent weight reductions up to –14.7% versus –2.3% with placebo. Gastrointestinal adverse events were common but mostly mild to moderate.
Two phase 3 trials are ongoing:
- ATTAIN-1 (NCT05869903) is a global trial enrolling 3000 participants with obesity or overweight plus comorbidities, evaluating body weight change over 72 weeks.
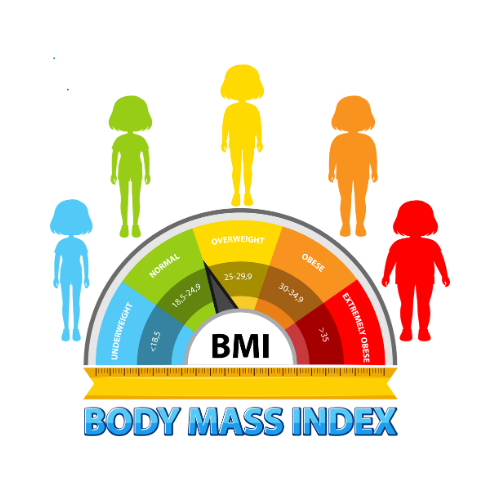
- ATTAIN-J (NCT05931380) is a Japan-specific trial for individuals with BMI ≥27–35 kg/m² with comorbidities, assessing weight loss and proportion achieving ≥5% weight loss.
1.2 Ecnoglutide
Ecnoglutide (XW003) is an engineered GLP-1 analog administered weekly via subcutaneous injection. A completed phase 2 trial compared weekly doses (1.2, 1.8, 2.4 mg) to daily liraglutide 3 mg over 26 weeks, but results remain unpublished.
A phase 3 trial (NCT05813795) is underway in China (n=664), targeting individuals with BMI >24 to <28 kg/m² with comorbidities, focusing on percent weight change and ≥5% weight loss over 72 weeks.
1.3 TG103
TG103 is a novel GLP-1/Fc fusion protein akin to dulaglutide, administered weekly. Phase 2 trials are ongoing in China comparing TG103 (15 mg, 22.5 mg) to placebo in 195 participants.
A phase 3 trial (NCT05997576) is evaluating TG103 (titrated up to 22.5 mg weekly) versus placebo for 40 weeks in adults with overweight or obesity and one cardiometabolic comorbidity, with completion expected by April 2025.
GLP-1 RA and Amylin Analog Combination
2.1 CagriSema
CagriSema combines cagrilintide, a long-acting amylin analog, with semaglutide, a GLP-1 RA. Amylin complements GLP-1 by promoting satiety, delaying gastric emptying, and modulating glucagon secretion.
In a phase 2 RCT (NCT04982575) among patients with type 2 diabetes, CagriSema induced greater weight loss (–15.6%) than cagrilintide alone (–8.1%) or semaglutide alone (–5.1%) over 32 weeks. HbA1c reduction was also superior.
Ongoing phase 3 trials:
- REDEFINE 1 (NCT05567796): A 3400-participant trial in the US and Europe, comparing CagriSema to semaglutide, cagrilintide, and placebo over 68 weeks.
- Two trials in Asian populations (NCT05813925, NCT05996848) focusing on weight loss efficacy.
- A head-to-head trial comparing CagriSema to tirzepatide (NCT06131437).
- REDEFINE 3 (NCT05669755): A cardiovascular outcomes trial enrolling 7000 participants to assess major adverse cardiovascular events (MACE).
Dual GLP-1 and Glucagon Receptor Agonists
3.1 Mazdutide
Mazdutide (IBI362, LY3305677) is a dual GLP-1/glucagon receptor agonist structurally related to oxyntomodulin, formulated for weekly injections. In phase 2 trials, mazdutide 6 mg resulted in –11.3% weight loss over 24 weeks, with preliminary data suggesting –15.4% weight loss at 9 mg.
Phase 3 trials include:
- NCT05607680 (n=600): Evaluating mazdutide titrated up to 6 mg over 48 weeks in individuals with BMI ≥28 kg/m² or ≥24 kg/m² with comorbidities.
- NCT06164873 (n=450): Focusing on individuals with BMI ≥30 kg/m², assessing weight change and ≥5% weight loss achievement.
Completion is expected in 2024 and 2025 respectively.
3.2 Survodutide
Survodutide (BI 456906) is another GLP-1/glucagon dual receptor agonist designed to enhance energy expenditure and reduce appetite. Preclinical and clinical data suggest glucagon receptor activation may improve hepatic metabolism, possibly benefiting patients with metabolic dysfunction-associated steatohepatitis (MASH).
A phase 2 trial in individuals with overweight and obesity showed up to –14.9% weight reduction with survodutide versus placebo at 46 weeks. In a phase 2 MASH trial, survodutide led to MASH resolution without fibrosis worsening in 83% of patients versus 18% with placebo (NCT04771273).
Ongoing phase 3 trials:
- SYNCHRONIZE-1 (NCT05970317) and SYNCHRONIZE-2 (NCT05987349): Global and China-focused trials evaluating weight loss and metabolic endpoints in adults with obesity over 76 weeks.
- SYNCHRONIZE-CVOT (NCT06289004): A cardiovascular outcomes trial enrolling 15,000 participants with obesity or overweight plus cardiovascular disease, examining MACE over several years.
- Additional trials (NCT06251128, NCT06269060, NCT06233744) are investigating survodutide’s impact on MASH, including histological endpoints and safety outcomes.
Discussion:
The expansion of GLP-1 RAs and novel dual agonists has revolutionized obesity pharmacotherapy, providing efficacious and increasingly tolerable options. Orforglipron’s oral formulation may improve accessibility, while CagriSema leverages amylin’s complementary effects on satiety and glycemic control. Dual agonists such as mazdutide and survodutide promise greater weight loss through synergistic increases in energy expenditure and reductions in hepatic fat, potentially addressing comorbid conditions like MASH.
However, challenges remain regarding long-term safety, particularly with dual agonists due to potential impacts on lean mass and amino acid metabolism. Head-to-head studies, such as those comparing CagriSema to tirzepatide, will clarify relative efficacy and safety profiles.
Conclusion:
A new generation of anti-obesity medications is poised to redefine obesity management. Agents in phase 3 development, particularly GLP-1 RAs, GLP-1/amylin combinations, and GLP-1/glucagon receptor dual agonists, show promise in achieving significant, sustained weight loss and cardiometabolic benefits. Ongoing trials will elucidate their role in clinical practice, particularly regarding cardiovascular risk reduction, hepatic outcomes, and long-term safety.
A new generation of anti-obesity medications is poised to redefine obesity management. Agents in phase 3 development, particularly GLP-1 RAs, GLP-1/amylin combinations, and GLP-1/glucagon receptor dual agonists, show promise in achieving significant, sustained weight loss and cardiometabolic benefits. For a deeper dive into complementary approaches that support medical treatment, visit this detailed guide on obesity and weight control solutions.
References:
- Pratt et al, 2023
- Wharton et al, 2023
- Guo et al, 2023
- Frias et al, 2023
- Ji et al, 2021, 2023
- Melson et al, 2024
- Hope et al, 2021, 2022
- Brouwers et al, 2024
- Romero-Gómez et al, 2023
- Additional trial identifiers as cited (e.g., NCT numbers)
You may have a slide presentation from here.
You may have supported data in excel sheet.